If you’re considering knee replacement surgery, understanding the procedure can make the experience less daunting and help set realistic expectations for recovery. While the thought of surgery may feel overwhelming, knowing what happens during the operation can provide clarity and confidence. Let’s take a detailed look at the steps involved in this life-changing procedure, along with practical tips to maximize your results.
Step 1: Making the Incision
The surgeon begins by making an incision along the front of your knee, typically 6–8 inches long. For minimally invasive techniques, the incision may be smaller. This step provides access to the joint, and the length of the incision will depend on your anatomy and the surgical approach chosen.
Step 2: Removing Damaged Tissue
Arthritis and injury damage the cartilage and bone in your knee joint, which the surgeon will carefully remove. Using precision tools, they prepare the ends of the femur (thigh bone) and tibia (shin bone), smoothing the surfaces to fit the new components. This step is crucial for proper alignment and long-term success.
Step 3: Positioning the Implants
Once the damaged tissue is removed, the new components are placed to restore function and stability.
-
Shaping the Bones: The ends of the femur and tibia are shaped to ensure the implants fit securely.
-
Metal Components:
-
Femoral Component: A metal cap replaces the end of the femur.
-
Tibial Component: A metal platform is secured to the tibia, often with a small stem for added stability.
-
-
Fixation:
-
Bone cement provides immediate stability for most patients.
-
Press-fit components are designed for younger, more active patients, allowing natural bone growth to secure the implants over time.
-
-
Plastic Spacer: An ultra-high molecular weight polyethylene (UHMWPE) spacer is placed between the metal components. This acts as a cushion, reducing friction and allowing for smooth, pain-free movement.
Step 4: Resurfacing the Patella (Optional)
The kneecap may be resurfaced with a polyethylene component to ensure smooth movement. However, not all surgeons perform this step, as it depends on your anatomy and the extent of damage to the patella.
Step 5: Closing the Incision
The procedure concludes with careful wound closure:
-
Suturing or Adhesives: Advanced techniques, including absorbable sutures or skin adhesives, are often used to minimize scarring.
-
Dressing: A sterile dressing is applied to protect the wound and promote healing.
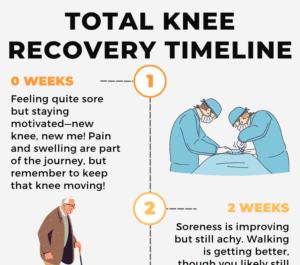
What to Expect Post-Surgery
While surgery is a significant step, recovery plays an equally vital role in achieving the best outcomes.
-
Pain and Swelling: Temporary discomfort and swelling are normal but can be managed with medications and physical therapy.
-
Rehabilitation: Most patients start walking with assistance within a day or two. A full recovery typically takes 3–6 months, with consistent rehab being key.
-
Longevity of Implants: Modern knee replacements last 15–20 years for most patients, with proper care and activity modifications.
Risks and Complications
Like any surgery, knee replacement carries some risks:
-
Infection: Keeping the incision clean and following your surgeon’s instructions can reduce this risk.
-
Blood Clots: Staying active and using prescribed blood thinners can help prevent this complication.
-
Stiffness or Reduced Range of Motion: Adhering to your rehab program minimizes this risk.
Preparing for Surgery: Tips for Success
-
Prehabilitation: Start strengthening exercises at least 3 months before surgery to build muscle and improve flexibility.
-
Weight Management: Every extra pound puts additional stress on your new joint. Losing weight before surgery can lead to better outcomes.
-
Nutritional Boost: Eat a balanced diet rich in protein, vitamins, and minerals to support healing.
-
Mental Preparation: Address anxiety and set realistic expectations by discussing your concerns with your healthcare provider.
-
Home Safety: Prepare your recovery space with assistive devices like grab bars and ensure clutter-free pathways for safety.
Therapeutic Edge
Knee replacement is not just a surgery—it’s a team effort that involves you, your surgeon, and your physical therapist. Understanding the procedure and committing to your recovery plan can make all the difference. By preparing your body and mind, you’ll set yourself up for the best possible outcome, regaining mobility and returning to the activities you love.