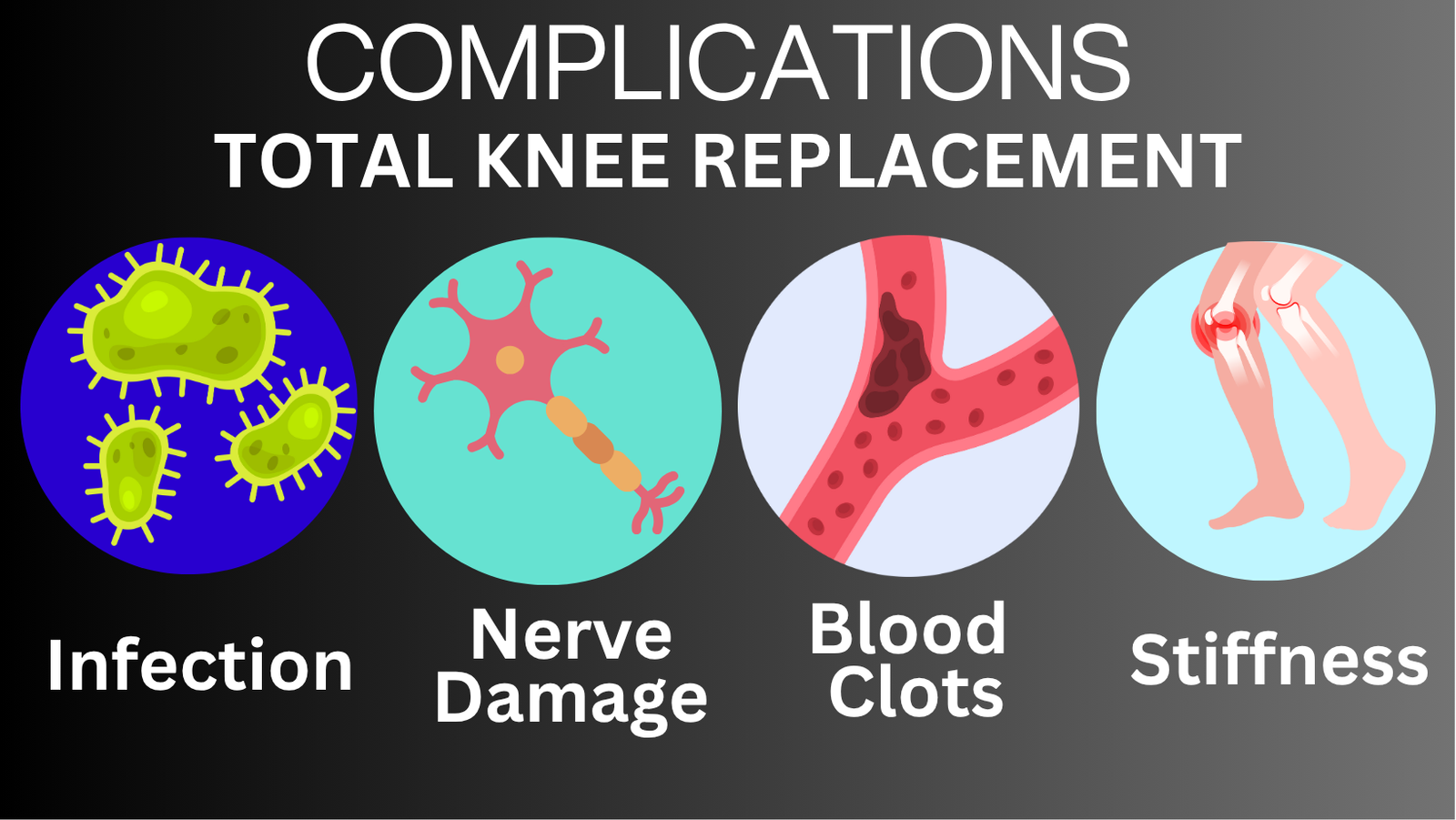
Knee replacement surgery can transform lives, providing relief from chronic pain and improving mobility. However, like any surgery, it comes with potential risks and complications. Understanding these challenges can help you navigate recovery with confidence and preparedness. Let’s explore some common post-surgery issues, their causes, and practical steps to mitigate them.
Infection: The Rare But Serious Risk
Infections after knee replacement surgery are uncommon, occurring in about 1% of cases, but they demand immediate attention.
What to Watch For:
-
Signs like fever, redness, swelling, warmth, or discharge from the incision site can indicate an infection.
How Infections Are Prevented:
-
Surgical Environment: Procedures are performed in ultra-clean operating rooms with filtered air to minimize contamination.
-
Antibiotics: Pre- and post-surgery antibiotics further reduce the risk.
Types of Infections:
-
Superficial Infections: These involve the skin and can often be treated with oral antibiotics.
-
Deep Infections: These are more severe, requiring surgical intervention, removal of the implant, and intensive antibiotic therapy.
Understanding Biofilms:
A protective layer of bacteria known as a biofilm can form on the implant, making infections harder to treat. This may necessitate removing the prosthesis and using a temporary spacer.
Who’s at Higher Risk?
-
Diabetes: Poorly managed blood sugar can impair wound healing.
-
Obesity: Extra weight stresses the joint and delays recovery.
-
Weakened Immune System: Conditions or medications that suppress immunity increase susceptibility.
-
Dental Health Issues: Poor oral hygiene can introduce bacteria into the bloodstream, increasing the risk of joint infections.
Nerve Damage: Rare but Noteworthy
While severe nerve damage is infrequent, minor nerve issues are relatively common.
Common Symptoms:
-
Numbness: Often temporary, it occurs near the incision and improves as nerves regenerate.
-
Neuromas: These painful nerve lumps may require injections or minor surgery for relief.
Preventive Tips:
Discuss your medical history with your surgeon to minimize nerve-related complications.
Blood Clots: A Common Concern
Blood clots, or deep vein thrombosis (DVT), occur in 40% to 80% of patients post-surgery but are often preventable with proper care.
Signs of a Blood Clot:
-
Pain, swelling, or redness in the leg.
Preventive Measures:
-
Compression Devices and Stockings: Enhance blood flow during and after surgery.
-
Early Mobilization: Walking shortly after surgery reduces clot risk.
-
Blood Thinners: Medications prescribed to prevent clot formation.
Your role in staying active and avoiding prolonged bed rest is critical for prevention.
Stiffness: Regaining Mobility
Knee stiffness, caused by excessive scar tissue buildup, can hinder recovery.
Key Strategies to Prevent Stiffness:
-
Begin moving your knee soon after surgery.
-
Stick to a pain management plan to stay active.
Treating Persistent Stiffness:
-
Manipulation Under Anesthesia (MUA): A procedure to break down scar tissue if stiffness persists.
-
Post-MUA Physiotherapy: Helps maintain motion and prevent recurrence.
Therapeutic Edge
Recovery from knee replacement surgery requires active participation. Here’s how to set yourself up for success:
-
Stay Active: Early mobilization not only prevents clots but also helps maintain flexibility and strength.
-
Monitor Symptoms: Be vigilant about infection signs, nerve pain, or unusual swelling.
-
Communicate with Your Team: Regularly update your surgeon and physical therapist on your progress or concerns.
-
Follow Rehabilitation Plans: Stick to your physiotherapy routine for the best functional outcomes.