Recover Faster. With Less Pain. Without Guesswork.
The Step-by-Step Total Knee Replacement Recovery System
Regain strength, mobility, and confidence with our guided recovery program after total knee replacement surgery.
✅ Know exactly what to do each day
✅ Progress safely without overdoing it
✅ Avoid common mistakes that slow recovery
✅ Build strength and confidence step-by-step
✅ Stop guessing if you’re doing “too much or too little”
Recovery Can Feel Overwhelming — You’re Not Alone
After knee replacement, most people aren’t short on motivation — they’re short on clarity.
❌ “Am I doing too much… or not enough?”
❌ “Why is my knee still stiff and sore?”
❌ “Am I behind where I should be?”
❌ “Am I hurting my new knee?”
The truth is: Most people don’t struggle because they’re lazy. They struggle because they don’t have a clear plan. And when you don’t have a plan, every workout feels like a guess.
This recovery system removes that uncertainty.

Your Recovery, Fully Mapped Out
So You Never Have to Guess What to Do

Step-By-Step Exercise Progressions
70+ guided progressions built from real clinic protocols — so you always know what comes next
Done-For-You Daily Plan
No planning. No confusion. Just open it and know exactly what to do today.
Soreness & Symptom Guidance
Learn how to train hard enough to improve — without flaring up or setting yourself back.
Built-In Progress Tracking
See your strength, motion, and confidence return week by week.
Your Recovery Journey
You’ll move through a structured, proven progression:
- Phase 1: Regain Motion & Reduce Swelling
- Phase 2: Restore Muscular Control & Mobility
- Phase 3: Build Strength and Power
- Phase 4: Return to Full Function
Designed by Orthopedic Physical Therapist Specialists
From the team at Therapeutic Edge
We help people recover from orthopedic surgery and injury every day.
This recovery system was built to give you the same structure, safety, and progression we use in the clinic — in a format you can follow at home, at your own pace.
✔ Board-Certified Orthopedic Physical Therapists
✔ Thousands of patients guided through recovery
✔ Evidence-based, clinically tested approach
Common Questions
If you’re unsure about anything, you’re not alone — here are answers to the most common questions we get.
Is this safe after knee replacement surgery?
Yes. This program was designed by orthopedic physical therapists who specialize in knee replacement rehab. The exercises and progressions follow the same principles used in high-quality physical therapy clinics.
You’ll also be given clear soreness and activity guidelines so you know when to push, when to hold steady, and when to back off — instead of guessing.
If you ever have new, worsening, or unusual symptoms, you should always check with your surgeon or healthcare provider.
What if I'm already in Physical Therapy?
That’s totally fine. This program can be used:
As a supplement to your in-person therapy
Or as a structured guide on days you’re not in the clinic
Many people use this to:
Better understand their rehab plan
Stay consistent between visits
And feel more confident about what they’re doing
If your therapist gives you specific restrictions, always follow those first.
What if I'm behind in my recovery?
You are not behind — recovery timelines vary a lot from person to person.
This program is phase-based, not calendar-based, which means:
You move forward based on what your knee can do
Not based on arbitrary dates
You’ll start in the phase that matches your current ability and progress from there.
How do I know if I’m doing too much or too little?
The program includes a soreness and symptom guide that teaches you:
What normal soreness feels like
What warning signs to respect
How to adjust your exercises and activity
This removes guesswork and helps you progress safely.
Do I need any special equipment?
No gym required.
Most exercises use:
Bodyweight
A chair, step, or wall
Light weights or resistance bands
You can do this at home.
How long do I have access?
You will have 12 months of access to the full program from the date of purchase.
This gives you plenty of time to:
Move through the entire recovery process
Revisit phases as needed
Use the program at your own pace
How long does the program take?
The full progression is designed to cover the entire recovery process, which for most people is 6+ months.
But remember:
You move based on your progress, not a fixed schedule
Some people move faster, some slower — both are normal
What if I’m not very strong or not very active?
That’s exactly who this is for.
The program:
Starts at a very approachable level
Builds gradually
Focuses on confidence, control, and tolerance — not “workouts”
You don’t need to be fit to start. You just need to be willing to be consistent.
Is this a replacement for medical care or physical therapy?
No.
This is:
A guided recovery program
An educational and exercise resource
It does not:
Provide medical diagnosis
Replace your surgeon or physical therapist
Manage complications
If you have concerning symptoms, you should always seek in-person medical care.
Do you offer refunds?
Because this program provides immediate access to all materials, we do not offer refunds.
Please read the page carefully and make sure this program is a good fit for you before purchasing.
If you have questions before buying, we encourage you to reach out first.
Want More Key Insights?
Explore expert guidance, recovery timelines, and common mistakes to avoid.
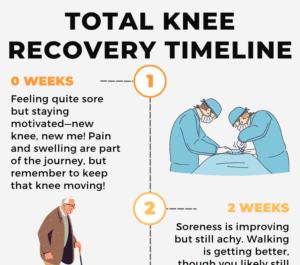
Total Knee Replacement Recovery Timeline: What to Expect
Recovering from a total knee replacement is a journey that requires patience, effort, and a clear understanding of what to expect at

Non-Medication Pain Relief Strategies: A Holistic Approach to Recovery
Managing pain after surgery doesn’t always mean reaching for a pill bottle. Non-medication pain relief strategies can be highly effective in reducing
Rehab and Recovery After Knee Replacement Surgery: Total Knee Do’s and Don’t
Recovering from a total knee replacement is a journey that requires patience, discipline, and the right strategies. While it might feel overwhelming
Key Details at a Glance
Expand each section for quick and accessible information about Total Knee Replacement rehab and recovery.
Surgery Overview
What to Know About Total Knee Replacement Surgery
Did you know that over 600,000 total knee replacement surgeries are performed annually in the U.S., with success rates exceeding 90%? For many, this life-changing procedure isn’t just about reducing pain—it’s about restoring freedom. Whether you’re struggling to climb stairs, enjoy a walk, or even sleep without discomfort, a knee replacement can offer relief when other treatments fall short. Studies reveal that most prosthetic knees last 15–20 years, and nearly 90% of patients report significant improvement in mobility and quality of life.
What Is Knee Replacement Surgery?
Think of total knee replacement as a reset for your joint. The procedure involves replacing damaged parts of your knee—typically worn-out cartilage and bone—with prosthetic components made of metal and plastic. These replacements are meticulously designed to mimic the natural motion and function of a healthy knee. With advancements in surgical techniques, recovery times have shortened, and outcomes have become increasingly predictable.
Why Consider This Surgery?
Knee replacement is primarily about reclaiming your mobility and relieving pain. Studies show that untreated knee arthritis can lead to a 20–25% decline in overall physical activity levels, increasing the risk of other health conditions like obesity and cardiovascular disease. If medications, injections, or physical therapy no longer provide relief and everyday activities feel insurmountable, it might be time to explore this option.
The Road to Recovery
A successful surgery is just the beginning. Recovery is a journey, and physical therapy plays a critical role in long-term success. While the joint itself is replaced, issues like muscle weakness or poor balance—often a result of years of joint degeneration—will still need attention. A structured rehab program can increase strength, improve flexibility, and enhance overall function. Patients who engage in consistent physical therapy report a 25% faster return to functional independence compared to those who don’t.
When Is Knee Replacement the Right Choice?
Understanding the “why” behind the surgery can help clarify whether it’s the right decision for you.
Common Reasons for Surgery:
- Osteoarthritis: The most common reason for knee replacement, affecting over 32.5 million Americans.
- Rheumatoid Arthritis: Chronic inflammation causing progressive joint damage.
- Traumatic Injury: Severe injuries compromising joint function.
Key Considerations:
- Pain Level: Is your pain constant, even at rest?
- Functional Limitations: Are simple tasks like walking, climbing stairs, or standing becoming increasingly difficult?
- Age: While replacements are more common in those over 55, younger candidates with severe conditions can also benefit.
What Can You Expect After Surgery?
The benefits of a total knee replacement extend beyond pain relief. Studies show that most patients achieve a 90–95% reduction in pain and significant functional improvements.
Expected Benefits:
- Mobility: Everyday tasks like walking and climbing stairs become much easier.
- Pain Relief: Say goodbye to constant, nagging discomfort.
- Quality of Life: Rediscover activities and hobbies you may have avoided for years.
Therapeutic Edge
Knee replacement surgery has the potential to be life-changing, offering freedom from pain and a renewed ability to move with confidence. But the surgery itself is only the first step toward reclaiming your mobility. Achieving the best possible outcome requires dedication to rehabilitation, patience through the recovery process, and a commitment to maintaining an active, healthy lifestyle. Success comes from teamwork—between you, your surgeon, and your physical therapist—all working together to ensure your new knee becomes the foundation for a brighter, more mobile future. With the right effort and support, your journey to a better quality of life can truly begin.
How to Prepare
Knee replacement surgery is a big step toward a pain-free life, but the path to recovery involves more than just the procedure itself. To ensure you get the best outcome, preparing ahead of time is crucial. Let’s explore the key factors that set the stage for a smoother recovery and long-term success.
Surgical Expertise
The skill of your surgeon can greatly impact your recovery. Minimally invasive techniques, for example, often lead to quicker healing and less discomfort. Be sure to research your surgeon’s experience with the latest procedures to maximize your outcomes.
Pre-Surgical Exercise
Did you know that knee arthritis can weaken the affected leg by up to 20%? Starting surgery with a weak leg can prolong recovery. Engaging in a pre-surgical exercise program can make a significant difference, helping you regain functional strength faster. Studies show that patients who prepare with structured exercises recover functional abilities 29% faster compared to those who don’t. Building strength and flexibility also lowers the risk of post-surgery complications and boosts overall fitness.
Weight Loss and Joint Health
Excess weight puts tremendous stress on your joints, especially the knees. Losing even a small amount of weight can have a profound effect. For every pound you shed, joint stress reduces by about 4 pounds—so losing 10 pounds reduces knee stress by 40 pounds! Weight management is vital, as obesity increases the risk of surgical complications by 30–40%.
Nutritional Boost
Your diet is your body’s fuel for healing. Protein is essential, as it can lower infection risk by 20% and speed up wound healing. Adequate Vitamin D levels also enhance bone health and reduce complications. Prioritize a balanced diet with plenty of vitamins, minerals, and lean proteins to support your recovery.
Post-Surgical Care
What happens after surgery is just as important as the procedure itself. Properly managing your incision and controlling pain are key steps in preventing complications. Follow your surgeon’s guidelines closely to set yourself up for a smooth recovery.
Rehabilitation and Physical Therapy
Rehab is your ticket to a strong and flexible knee. Sticking to your physical therapy plan is crucial, as these exercises help rebuild strength and mobility. With commitment, you can return to daily activities with confidence and ensure long-term success.
Mental Readiness
Your mindset can significantly influence your recovery. Patients with a positive outlook have a 25% faster recovery time and better adherence to their rehab programs. Knowing what to expect and addressing any concerns with your healthcare provider can reduce anxiety and enhance your healing process.
Home Preparation
A safe, accessible home environment is essential for recovery. Falls are a leading cause of complications post-surgery, occurring in up to 10% of patients within the first three months. Take steps to prepare your home with assistive devices and a clear, hazard-free setup to avoid setbacks.
Therapeutic Edge
Preparation for knee replacement surgery isn’t just about checking boxes—it’s about creating a foundation for long-term success. By focusing on prehabilitation, maintaining a healthy weight, prioritizing nutrition, managing your mental well-being, and ensuring a safe recovery environment, you are actively shaping your outcome. Research shows that these steps collectively lead to faster recovery, fewer complications, and a smoother return to daily life.
Immediate Recovery
Undergoing total knee replacement is a transformative step toward a pain-free life, but the immediate recovery period is pivotal in setting the foundation for your long-term success. Knowing what to expect and how to navigate this phase will empower you to take control of your healing process and achieve the best outcomes. Here’s a comprehensive guide to help you make the most of your first steps post-surgery.
The First 24-48 Hours: Prioritizing Pain Management and Mobility
Effective pain management is key to a smoother recovery. Approximately 85% of patients experience manageable pain levels with a combination of prescribed medications and non-pharmacological methods such as ice therapy and elevation. Following your doctor’s recommendations will allow you to stay on track with early rehab exercises—essential for preventing stiffness and promoting mobility.
Early Dos and Don’ts: Building Healthy Recovery Habits
The Do’s for Immediate Recovery
Take Your Pain Medication
Pain management isn’t just about comfort—it’s essential for progress. Follow your doctor’s instructions to stay ahead of the pain, which will allow you to participate fully in your rehab exercises and daily activities.Move Your Knee Regularly
Stick to your prescribed exercises and stretches to avoid stiffness and encourage circulation. Small, consistent movements can make a big difference. Think of rehab as a daily investment in your mobility.Ice and Elevate
Swelling is a normal part of recovery, but icing and elevating your leg above heart level can help. Aim for 15-20 minutes with an ice pack several times a day to minimize discomfort and promote healing.Fuel Your Recovery
A balanced diet and proper hydration are your body’s tools for repair. Focus on lean proteins, whole grains, fruits, and vegetables to reduce inflammation and speed up healing.
The Don’ts for Immediate Recovery
Don’t Rest with a Pillow Only Under Your Knee
While it may feel comfortable, this position can lead to stiffness. Instead, keep your leg in a neutral position, or support the entire leg if your doctor recommends it.Don’t Ditch Your Assistive Devices Prematurely
Walkers, crutches, or canes are your allies in recovery. They prevent falls and reduce strain on your new joint. Transition only when your physical therapist says it’s safe.Don’t Sit for Long Periods
Extended sitting can lead to swelling and stiffness. Incorporate gentle stretches and short walks into your day to keep your knee flexible and mobile.Don’t Smoke or Overindulge in Alcohol
Both smoking and excessive drinking can hinder healing. Focus on creating a recovery-friendly environment for your body.
Non-Medication Pain Management Strategies
While pain medications are essential, incorporating non-pharmacological approaches can enhance your comfort and recovery.
Ice Therapy: Reduces swelling and provides localized pain relief. Use for 15-20 minutes, several times daily.
Elevation: Keeps swelling down by promoting circulation. Use pillows or recliners to keep your leg elevated above heart level.
TENS Units: Offers targeted pain relief by sending mild electrical impulses to nerves. Consult your provider for guidance.
Massage Therapy: Improves circulation and reduces tension. Ask your physical therapist to show you safe, effective techniques.
Mind-Body Techniques: Deep breathing, mindfulness, or meditation can help you manage stress and discomfort naturally.
Nutrition and Hydration: Fueling Your Recovery
Eating a balanced diet rich in protein, vitamins, and anti-inflammatory nutrients accelerates healing. Studies show that consuming adequate protein can improve surgical wound healing rates by 20%. Staying hydrated supports circulation and tissue repair, reducing the risk of complications like blood clots.
Assistive Devices and Wound Care: Ensuring a Safe Start
Using walkers or canes as recommended helps distribute weight evenly, preventing strain on your healing knee. Proper wound care, including keeping the incision clean and dry, reduces the infection risk significantly, which occurs in less than 1% of cases when care instructions are followed meticulously.
Therapeutic Edge
Immediate recovery is about balance: managing pain, staying active, and giving your body what it needs to heal. Here are the big takeaways to remember:
Stick to your rehab plan. Progress comes from consistency.
Pain is normal but should never hold you back from moving forward. Manage it proactively.
Healthy habits like proper hydration, nutrition, and quitting smoking can significantly accelerate healing.
Patience is key—recovery is a marathon, not a sprint. Celebrate small victories along the way!
By focusing on these principles, you’ll set yourself up for a smoother recovery and a stronger, more mobile future.
Rehabilitation
Recovering from a total knee replacement is a journey with highs and lows, but understanding the process can help you stay prepared and motivated. Partnering with your healthcare team is essential, and remember: recovery is a marathon, not a sprint. Here’s a stage-by-stage guide to help you anticipate milestones, manage expectations, and navigate the recovery process.
0-2 Weeks: Getting Started
What to Expect:
Pain and Swelling: Expect significant discomfort and swelling initially. Your doctor will provide medication to help manage these symptoms.
Mobility: You’ll likely need a walker, crutches, or a cane to move around. Simple exercises guided by your physical therapist will keep your knee from stiffening.
Incision Care: Follow your surgeon’s instructions to keep the incision clean and dry to prevent infection.
Milestones:
Basic Movement: Start with gentle exercises like ankle pumps and heel slides to encourage circulation and mobility.
Getting Up and About: Gradually walk short distances around the house with assistance.
How You Might Feel:
Sore and Tired: Fatigue and soreness are normal. Rest is essential, but short, purposeful movements will aid recovery.
2-6 Weeks: Early Recovery
What to Expect:
Pain and Swelling: Both should begin to subside with consistent use of ice packs, elevation, and pain management strategies.
Mobility: You’ll become more confident moving around. Many patients transition from crutches to a cane during this phase.
Milestones:
Walking Progress: You’ll start walking with less assistance and greater ease.
Improved Range of Motion: Physical therapy will focus on bending and straightening your knee, working toward functional movement.
How You Might Feel:
Better and Encouraged: With less pain and improved mobility, your confidence will grow as you notice progress.
6-12 Weeks: Mid-Recovery
What to Expect:
Pain and Swelling: Both are minimal, with occasional discomfort managed by over-the-counter medications.
Mobility: You’ll likely walk unassisted, and exercises will become more challenging to build strength and flexibility.
Milestones:
Regaining Independence: Resume daily activities like light household chores and possibly driving, depending on your recovery pace.
Strength and Flexibility Gains: Advanced exercises will help restore functionality and stability in your knee.
How You Might Feel:
Energized and Active: With increased strength and mobility, you’ll feel more capable of tackling everyday tasks and light activities.
3-6 Months: Later Recovery
What to Expect:
Pain and Swelling: These should be nearly gone, although some discomfort during high-impact activities is normal.
Mobility: You’ll likely regain a natural walking pattern and participate in more varied physical activities.
Milestones:
Resuming Normal Activities: Return to work, hobbies, and other routines you enjoyed before surgery.
Full Range of Motion: Near-complete range of motion and strength in your knee should be achieved.
How You Might Feel:
Confident and Strong: By this stage, you’ll feel significant improvements and be ready to fully enjoy life with minimal limitations.
6+ Months: Long-Term Recovery
What to Expect:
Pain and Swelling: Most patients report little to no pain and have full mobility by this point.
Mobility: You’ll have the strength and flexibility to handle a wide range of activities, including light sports.
Milestones:
Full Recovery: You should feel completely recovered and ready to take on more strenuous activities.
Ongoing Strengthening: Regular exercises will help you maintain your progress and prevent future issues.
Therapeutic Edge
Recovery Timelines Are Unique but Predictable
While the exact timeline varies for everyone, the key to steady progress lies in consistency. Sticking to your recovery plan ensures gradual but meaningful improvements, no matter how your body heals.Pain and Stiffness Are Part of the Process
Discomfort during recovery is normal and expected, but don’t let it discourage you. Effective pain management, coupled with prescribed mobility exercises, helps you overcome these challenges and keeps you moving forward.Celebrate Every Milestone
Each achievement, no matter how small—whether it’s your first independent step or returning to a cherished activity—is a testament to your effort and resilience. Acknowledge and celebrate these victories as markers of your progress.Your Recovery Is as Unique as You Are
No two journeys are the same, but with patience, persistence, and support from your healthcare team, you’ll achieve your goals. Focus on the big picture: regaining the mobility and quality of life you deserve.